|
It was a couple of days before Cathie could go see her. she went just
as soon as she was able. I stayed out of work, tending to Cathie, and we
spent every available minute in NICU. It did not take us very long to fall
in love with Elizabeth. Cathie had wanted to breastfeed, but the circumstances
prevented it. Instead, she pumped, and pumped and pumped, and the milk
was tested. When it was safe for Elizabeth, they began to give her Mom's
milk in addition to her special formula.
Various tests were always being run. Elizabeth was diagnosed as having
a PDA, which is not uncommon in premature babies. This was treated with
drugs and corrected. She also had tachycardia, an unexplained racing of
the heart. She stayed on medication for that for about 6 months. But more
serious news came to us near the end of the third week: the doctors had
discovered internal bleeding in Elizabeth's brain. The bleeding had stopped,
they said, but they had been monitoring the pressure in Elizabeth's brain,
and it was increasing. A shunt would have to be installed.
I gave permission for the surgery, which was to take place right away.
All I remember is waiting in the waiting room for a long time. Finally,
a doctor came out, and told me that Elizabeth had come through the surgery
fine, and that it was a success. As he explained the procedure to me, it
was apparent that he was in fact the neurosurgeon who had performed the
operation. When he finished explaining everything, and asked if I had any
questions, I said, "Yeah. How old are you, anyway?" He said he
was 36.
A shunt is a device which consists of a tube which is inserted into
the center of the brain, where the brain fluid is produced. It is necessary
when the brain fluid, which normally bathes the brain, carrying any dead
cells with it, cannot get out of the head as fast as it is being produced.
In Elizabeth's case, the bleeding from the brain probably blocked the normal
path down the spinal column. As the blood clotted and dried, scar tissue
formed around it, narrowing or closing the tiny spinal canal opening. It's
like a faucet turned on in a sink with a slow drain. Anyway, the tube passes
through a part of the brain which is not used, into the center. The end
in the brain is left open. The other end attaches to a pressure valve which
sits under the scalp. Another tube runs from the valve, under the skin,
all the way down her neck, down her chest, and ends up in her abdominal
cavity. This is where the fluid normally exits the spine and is absorbed
into the body and eliminated. They left a lot of extra tubing so that as
she grows, the tubing will uncurl and she won't have to have the whole
system replaced. She will have the shunt all of her life, although she
may actually outgrow the need for it to function at some point. Shunts
are mechanical devices, and 50% of them fail in the first 5 years and must
be replaced. Other than watching for signs of shunt failure (intense vomiting,
severe headaches) no special treatment is necessary. Elizabeth goes for
regular CT scans, about every six months (now every year) to make sure
everything is still working properly.
In NICU were approached by a doctor one day who introduced himself to
us, said he was a plastic surgeon, and would like to take Lizzie's case.
Since we did not know any doctors, or how we would even begin to line up
all the necessary procedures, we were grateful for his assistance. After
a brief consult in NICU, he left, and when he was gone half a dozen nurses
came rushing over and asked if we knew who he was. "No, why, did we
make a mistake? ," I asked. They said that he was one of the top people
in his field - Rami Kalus - and we were extremely lucky to have him!
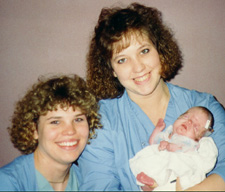 Time passed quickly
while Lizzie was in NICU, and Cathie and I got used to the routine of staying
with her from early in the morning until late at night. She had occasional
spells of tachycardia, an unexplained racing of the heart. Sometimes her
heartbeat would go off the scale of the monitor (200) but this was controlled
by medications. We began to feel comfortable with the situation, growing
to love our Lizzie and her nurses more every day. The nurses there at NICU
really helped us a lot, and Lizzie was their pet. They took pictures of
her for us when she would do something cute. They would call us just to
let us know everything was ok. Time passed quickly
while Lizzie was in NICU, and Cathie and I got used to the routine of staying
with her from early in the morning until late at night. She had occasional
spells of tachycardia, an unexplained racing of the heart. Sometimes her
heartbeat would go off the scale of the monitor (200) but this was controlled
by medications. We began to feel comfortable with the situation, growing
to love our Lizzie and her nurses more every day. The nurses there at NICU
really helped us a lot, and Lizzie was their pet. They took pictures of
her for us when she would do something cute. They would call us just to
let us know everything was ok.
Lizzie never did like the breathing tubes, which had been in her since
birth. She did her best to get them out, succeeding on more than one occasion.
She was stubborn from day one, clinging to life and fighting every time
she was disturbed from her comfort zones. It got to the point where she
had to be restrained to keep her from pulling out her breathing tube. One
day, the phone rang about 6 am - it was NICU - and of course we panicked.
Lizzie was all right - but she had taken out the breathing tube, very quietly,
and laid there breathing on her own before being discovered! The nurses
were so excited they had to call us - they said since she was doing so
well, the doctors had decided to leave it out and let her breathe on her
own to see how she did, and she was doing very well.
Back Top
Next
|